Epigraph Vol. 17 Issue 3, Fall 2015
Classifying Seizures in the Very Young: Initial Plans of the Neonatal Seizure Task Force (part of ILAE Commission on Classification & Terminology)

Seizures are the most common neurological emergency in the neonatal period and are associated with considerable mortality and morbidity. Neonatal seizures are usually acute and often subclinical. They may show discrete clinical manifestations that are often difficult to differentiate from movements seen in sick preterm or term babies. Hence, the need for EEG confirmation for the diagnosis of neonatal seizures is now widely accepted. All of this makes the integration into a classification serving all ages difficult, which is reflected by the fact that, until recently, the ILAE classifications did not include neonatal seizures.
Consequently other classifications have been published by neonatologists and paediatric neurologists, that are specific to the neonatal period (Volpe, 1989; Mizrahi and Kellaway, 1987). A recent survey at the 9th international conference of brain monitoring and neuroprotection in the newborn (Cork, 2015) has shown that most neonatologists either do not classify neonatal seizures or use the Volpe classification. Although simple to use, this classification has the disadvantage that it is based purely on clinical manifestation and disregards the need for EEG diagnosis, consequently subclinical seizures are ignored and many non-seizure events are classified as seizures.

Although there are a number of single centre studies to describe seizure semiology with EEG (Watanabe et al. 1977; Mizrahi and Kellaway, 1987; Nagarajan et al. 2012), no multicentre collaboration has so far come to a consensus on how best to define, characterise and classify/organise neonatal seizures.
The development of a new classification for epilepsy has been the major focus of the ILAE Commission on Classification and Terminology over the last few years. One of the aims of the new classification of the epilepsies was to have unifying concepts for seizures for all ages and thus “neonatal seizures are no longer regarded as a separate entity. Seizures in neonates can be classified within the proposed scheme.” However this position is controversial, as it does not take into account the particular complexities in this age group including acute aetiologies, high electrographic seizure burden and management within the intensive care setting. In 2014, a new Task Force on Neonatal Seizures was established with the assignment to develop ways in which neonatal seizures and epilepsies can be integrated into the new classification of the epilepsies.
At that time a set of guiding principles was established for the new classification. The classification should address seven key points.
- Take into account the specificities of seizures at different gestational ages. The developing brain changes rapidly and how it will support seizures will change considerably over several weeks.
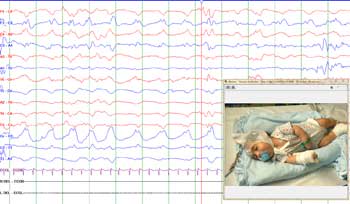
- Be based on electro-clinical phenotyping. There are many behaviours that are seen in a premature or sick neonate that are difficult to classify on clinical appearance alone. Physiological confirmation is needed.
- Reflect the pathophysiological origin / aetiology of events. The prognosis of a child with neonatal seizures is related to the cause.
- Emphasise the key role of EEG in the diagnosis of neonatal seizures. Patterns on recordings vary with age, and there must be consensus on what patterns constitute seizures so that suspicious behaviours can be identified as seizures.
- Have implications for the management and treatment of events. It is important to determine which treatments under specific situations will be beneficial.
- Be acceptable to epileptologists, neonatologists, paediatricians and neurologists alike. To be useful in providing a common language for clinicians treating neonates all parties have to agree that it is a useful approach.
- Be applicable in all health care settings. A classification is not useful if it can only be applied at a limited number of facilities.
A meta-analysis of electro-clinical semiology of term and preterm seizures is being prepared as a point of reference. We are currently working on a diagnostic framework to describe neonatal seizures which can be used in conjunction with the new classification of the epilepsies using the same concepts and terminology. This will be verified via a retrospective collection of clinical and video-EEG data on seizures in neonates of different gestational ages for electro-clinical phenotyping.
Task Force members: Ronit Pressler (Chair), Sameer Zuberi, Elissa Yozawitz, Perrine Plouin, Roberta Cilio, Magda Nunes, Sampsa Vanhatalo, Eli Mizrahi, Nico Moshé (Management Committee Liaison).
References
Nagarajan L, Palumbo L, Ghosh S. Classification of clinical semiology inepileptic seizures in neonates. Eur J Paediatr Neurol. 2012 Mar;16(2):118-25.
Mizrahi EM & Kellaway P. Characterization and classification of neonatal seizures. Neurology 1987;37:1837-44.
Volpe JJ. Neonatal seizures: current concepts and revised classification. Pediatrics, 1989;84:422-8
Watanabe K, Hara K, Miyazaki S, et al. Electroclincal studies of seizures in the newborn. Folia Psychiatr Neurol Jpn 1977; 31:381-92.
Subscribe to the ILAE Newsletter
To subscribe, please click on the button below.
Please send me information about ILAE activities and other
information of interest to the epilepsy community