Epigraph Vol. 18 Issue 2, Fall 2016
A Population Based Strategy for Comprehensive Epilepsy Care in Ontario, Canada

Ontario has 95,000 people with epilepsy, 15,000 of whom are children. As is true everywhere else in the world, about one-third of these people (30,000-35,000) have medically refractory epilepsy. Also as is true throughout the world, prior to 2013 the care that Ontarians with epilepsy received was uneven and their access to surgical evaluation varied from capricious to non-existent, even in the face of a very good single-payer health care system.
There were several reasons for this situation, including a lack of awareness amongst primary care providers and neurologists of the value of epilepsy surgery, as well as a patchwork referral pattern for those patients with uncontrolled seizures. Further, there was a major lack of understanding in the government of the scope of the problem of epilepsy in Ontario, about the role of epilepsy surgery and its value in reducing the burden of illness, and the costs of epilepsy to the system. Finally, there was the problem of geography. The majority of people in Ontario live in the southern part of the province, so services are sometimes difficult to provide to the far-flung regions of Northern Ontario (Figure 1). Since 2013, the Ontario Ministry of Health and Long Term Care [MOHLTC] has taken on these challenges and established the first population-based strategy for comprehensive epilepsy care in North America.
Figure 1. Map of Canada. The red arrow points to the approximate division between Southern Ontario, where most of the population and medical resources are, and the large expanse of Northern Ontario, with a lower population density and more widely dispersed health care facilities.

Ontario guidelines and supporting information
Comprehensive epilepsy care in Ontario
In response to an expert panel report on epilepsy care in the Province of Ontario in 2011, the MOHLTC regionalized epilepsy care with the establishment of Adult and Pediatric District Epilepsy Centers (DEC) and Adult and Pediatric Regional Epilepsy Surgery Centers of Excellence (RESCE) in 2013. As well, the MOHLTC created an Epilepsy Implementation Task Force [EITF] to develop an integrated system for epilepsy care in Ontario. The EITF brings together senior clinicians and administrators from the Ontario epilepsy community to improve access by coordinating resources and wait lists, establishing standardized diagnostic and surgical protocols across centres, and developing support for primary care providers. As part of this mandate, the EITF has created a series of Provincial Guidelines for primary care providers and community neurologists. (LINKS TO PAPERS ON ILAE PAGE)
In addition, the EITF was asked to develop educational programs for primary care providers and community neurologists. The Ontario EITF set the criteria for a comprehensive epilepsy program (CEP) of integrated care for the management of individuals with epilepsy within a multidisciplinary team. The CEP covers various aspects of care, including medical (epileptologists), psychosocial (social workers and neuropsychologists) and skilled epilepsy nursing care (nurse practitioners). The pProgram also covers nutritional management (dietitian) and appropriate neurodiagnostic investigations. The latter includes all hardware and personnel for neuroimaging and neurophysiology, including an EMU with protected beds, capability for presurgical diagnostic evaluation, and established links to Community Epilepsy Agencies. Full infrastructure is provided within the system for surgical management of appropriate candidates.
The District Epilepsy Centre (DEC) houses a comprehensive epilepsy program that provides all appropriate epilepsy-related clinical services except for epilepsy surgery. A DEC provides basic investigations necessary to determine candidacy for epilepsy surgery, including assessment by an epileptologist, and full EMU capability, including neuropsychological evaluations. The Regional Epilepsy Surgery Centre of Excellence (RESCs) also houses a comprehensive epilepsy program that provides all the services available in a DEC, with the addition of all necessary facilities for state-of-the-art epilepsy surgery.
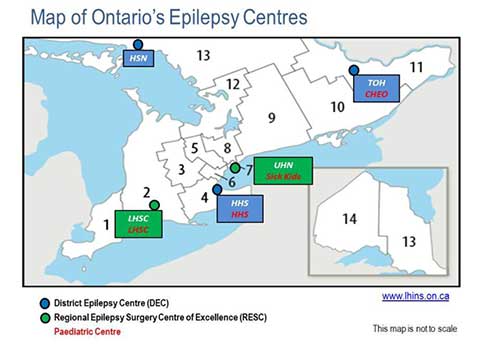
Figure 2. DEC hospitals include Health Sciences North in Sudbury [both adults and children], an adult DEC at Hamilton Health Sciences Centre, a pediatric DEC at Hamilton Health Sciences Children’s Hospital, an adult DEC at the Ottawa Hospital, and a Pediatric DEC at Children’s Hospital of Eastern Ontario. Current RESCs are London Health Sciences Centre [Adult and Pediatric], Hospital for Sick Children [Pediatric], and University Health Network (Toronto Western Hospital – Adult].
How the system works
Where possible, anyone with new onset of epilepsy will be referred by their primary care provider to a neurologist who will obtain an EEG and make first-line treatment recommendations to be managed by their primary care provider. Those patients who failed to respond to a conventional first-line anticonvulsant medication, or who had complex epilepsy from the onset (such as multiple or frequent seizures or status epilepticus) are referred to the DEC where appropriate medical management recommendations are developed, psychosocial support provided, and a connection with local community epilepsy agencies established. A preliminary evaluation of a patient's candidacy for epilepsy surgery is made at the DEC, and, if the patient is a candidate for surgery, he/she is referred to a RESC for further evaluation.
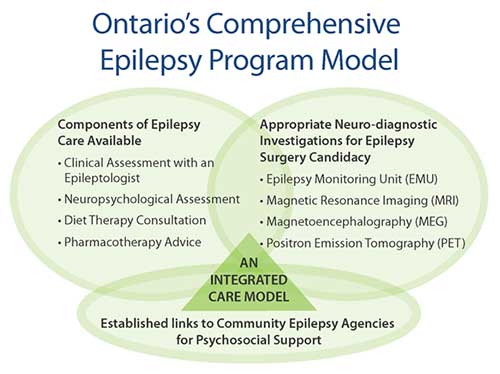
Figure 3. The Ontario Comprehensive Epilepsy Program Organization: How a patient can move through the care system
How did we engage government?
In 2007, the Ontario Health Technology Advisory Committee (OHTAC) reviewed functional brain imaging modalities and made a recommendation to examine the use of magnetoencephalography (MEG) in the determination of surgical candidacy in children with medically refractory epilepsy. The results of this field evaluation [see Lim M, et al. Epilepsy Res 2013;107:286-96] were then presented to OHTAC in January 2011. A subsequent expert panel recommended in August 2011 that Ontarians of all ages who suffer from epilepsy should have universal access to quality, evidence-based, comprehensive medical and surgical epilepsy care at the right time and in the right place.
Further, the expert panel determined that epilepsy care in Ontario at that time left much to be desired. At that time, a child or adult with new onset epilepsy would most likely be seen initially either in the Emergency Department or by a primary care provider with no standardized approach to diagnosis and treatment. If the seizures subsequently declared themselves as medically refractory, the patient may or may not have been referred for a surgical evaluation. There was no support system for patients and their families, nor were there evidence-based clinical guidelines in place regarding medical or surgical treatment. The expert panel pointed out that, based on the sheer numbers of patients with epilepsy and their impact on the health care system, epilepsy was a major public health issue in Ontario which, to date, had been inadequately addressed. The expert panel further opined that the major reasons for this state of affairs was a problem in attitude and awareness amongst physicians, including neurologists, who care for these adults and children with epilepsy, appropriate allocation of resources, and geographic problems given the huge sprawling size of the province. The expert panel made a number of recommendations that were adopted by the MOHLTC and led to the new provincial comprehensive epilepsy strategy. (LINK TO RECS ON ILAE WEB PAGE)
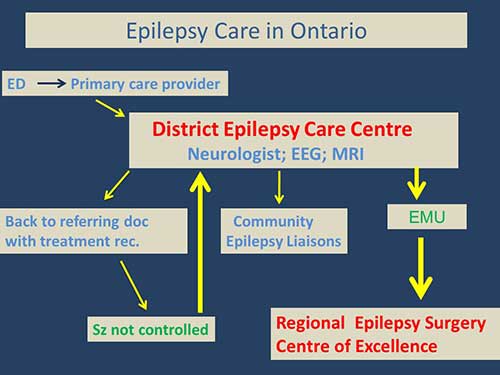
Figure 4. The services provided by the components of the Ontario Comprehensive Epilepsy Program.
Why these efforts have succeeded so far
- Ontario has an evidence-based system for the evaluation of proposed programs for MOHLTC funding, and the data about the burden and costs of epilepsy in the province supported the panel’s recommendations.
- The involved hospitals, professional providers of epilepsy care in Ontario, and the community epilepsy agencies supported the recommendations.
- The government funded all of the infrastructure for the DECs and RESCs and provided the administrative infrastructure to make the plan happen. The government’s desire to improve access to epilepsy surgery throughout the province led to the EITF’s designation as a subgroup of Provincial Neurosurgery Ontario (PNO), a provincial committee working to develop a comprehensive neurosurgical system. The EITF works with PNO to support equitable and timely access to neurosurgical care, including epilepsy surgery, and to help maintain the province’s neurosurgical capacity. The administrative support for all of the work of EITF, without which none of this would have happened, is supplied by the Ministry through Critical Care Services Ontario (www.criticalcareontario.ca).
- It is absolutely critical for anyone who wishes to emulate our success to memorize the following sentence: The main reason we were successful is that we put a face to epilepsy in every presentation to government. Jim Bowen from the PATH group at McMaster University and I made virtually every presentation to multiple government agencies within MOHLTC, from our initial presentation to OHTAC in March 2011, to our final presentation to senior managers of MOHLTC in the winter of 2012. In every single presentation we made over the two years it took us to get this initiative funded, I always presented the same patient, Anthony, a young boy with medically refractory localization-related epilepsy who was cured by epilepsy surgery. Each presentation of Anthony always met with the same result – everyone in the room was blown away by the human tragedy of epilepsy, by what Anthony and his family had to deal with, and by the thrill of a dramatic surgical success in a child with medically refractory epilepsy and the hugely positive impact on Anthony’s life occasioned by this outcome. It was Anthony who got us where we are today.
Ontario guidelines and supporting information
- Epilepsy Care in Ontario: An Economic Analysis of Increasing Access to Epilepsy Surgery (2012)
- Provincial Epilepsy Monitoring Unit (EMU) Guidelines for Ontario (Jan 2014)
- OHTAC Recommendation: Care for Drug-Refractory Epilepsy in Ontario (Ontario Health Technology Advisory Committee) (2012)
- Epilepsy Surgery: An Evidence Summary
- Diagnostic evaluation of infants, children, and adolescents with epilepsy for surgery candidacy and the role of magnetoencephalography (MEG)
- Provincial Guidelines for Epilepsy Surgery Referrals in Ontario (2016)
- Provincial Guidelines for regional epilepsy Surgery Centres (2016)
- Provincial Guidelines for the Management of Epilepsy in Adults and Children (2015)
- Provincial Guidelines for the Management of Medically-Refractory Epilepsy in Adults and Children who are not Candidates for Epilepsy Surgery (2016)
- Regional Epilepsy Surgery Centres - Program Model and Technical Guide (2016)
Subscribe to the ILAE Newsletter
To subscribe, please click on the button below.
Please send me information about ILAE activities and other
information of interest to the epilepsy community