
34th International Epilepsy Congress
Virtual Congress
28 August - 1 September 2021
Programme
The ILAE, the IBE, and the Scientific and Organising Committee are delighted to be able to offer you the best in epilepsy education.
View IEC 2021 Programme with sessions, dates and times
View IEC 2021 Programme Schedule as a PDF
The congress will present the highest quality, flexible education, providing a platform to hear from world-renowned experts and with the on-demand recordings of the sessions allowing you to attend sessions at your own convenience. All of the content will be accessible for delegates during and after the congress. Sessions will facilitate interaction by asking questions, sharing your opinion, participating in polls, and more.
The congress programme comprises plenary lectures, interactive sessions, specialty sessions and a comprehensive teaching programme.
Further details of sessions may be found in the sections below.
INTERACTIVE PROGRAMME PLANNER
Full details of the congress programme are available in the online planner.
View the Interactive Programme Planner
You can browse the entire scientific programme, search for sessions, chairs and speakers and create your own personal itinerary by selecting your favourite sessions. You can also download the programme for any session.
Start building your own itinerary – simply access the Planner and click on the calendar icon in the top right corner of the session of your choice to download a calendar invite.
Presidential Symposium: The future of epilepsy care: best practices
Co-chairs: Samuel Wiebe (Canada) & Martin Brodie (Scotland)
- Welcome – Martin Brodie (Scotland)
- Responsible telemedicine in epilepsy: challenges and best practices – Josephine Chan (Australia)
- Wearables in epilepsy: what is their role in telemedicine? – Sándor Beniczky (Denmark)
- Using videos of patient-recorded seizures: The future for seizure diagnosis? – Sameer Zuberi (United Kingdom)
- Patient-reported outcome measures in telehealth: an untapped resource for patient care? – Nathalie Jette (USA)
- Real world evidence and the patient experience: are we doing it right? – Francesca Sofia (Italy)
- Panel discussion
Choosing wisely – needs and reality in patient care
Co-chairs: Mary Secco (Canada) & Kette Valente (Brazil)
- Ongoing information and support needs across the lifespan – Mary Secco (Canada)
- Strategies to improve health literacy – Francesca Sofia (Italy)
- Beyond seizure control: thinking outside the box – Kette Valente (Brazil)
- Choosing wisely in resource-restricted settings – Symon Kariuki (Kenya)
Cutting edge diagnostic methods in epilepsy: seizure onset zone
Co-chairs: Fabrice Bartolomei (France) & Hui Ming Khoo (Japan)
- From quantification to modelling of the seizure onset zone – Julia Scholly (France)
- The role of neuroimaging in the definition of the seizure onset zone – Fernando Cendes (Brazil)
- What role for subcortical regions in the genesis and propagation of focal seizures? – Ren Liankun (China)
- How HFO and spikes may help to define the seizure onset zone – Julia Jacobs (Canada)
Epilepsy genetics: a global perspective
Co-chairs: Holger Lerche (Germany) & Iscia Lopes-Cendes (Brazil)
- Overview and clinical implications of genetic findings – Heather Mefford (USA)
- Role of common and rare genetic variants – Gianpiero Cavalleri (Ireland)
- Genetic informatics for the busy clinician – now and the future – Ingo Helbig (USA)
- Perspectives of gene therapy – Steven Petrou (Australia)
Epilepsy surgery 2021 – state-of-the-art
Co-chairs: Philippe Ryvlin (Switzerland) & Lara Jehi (USA)
- Introduction with Survey #1 (3 questions) – Lara Jehi (USA)
- Non-invasive investigations: the optimal work-up – Eugen Trinka (Austria)
- State-of-the-art StereoEEG: when, why and how – Philippe Ryvlin (Switzerland)
- Survey #2 (3 questions) – Lara Jehi (USA)
- MRI-guided laser-ablation: indications and outcomes – Michael Sperling (USA)
- Epilepsy surgery in limited-resources settings: is it really different? – Jayanti Mani (India)
- Is there a future for epilepsy surgery? YES – Caroline Neuray, ILAE-YES (United Kingdom)
- Questions and conclusion – Philippe Ryvlin (Switzerland)
Is epilepsy a progressive neurodegenerative disease?
Co-chairs: Marian Galovic (Switzerland) & Mark Keezer (Canada)
- Mental decline in chronic epilepsy: fact or fiction? – Christoph Helmstaedter (Germany)
- Progressive neurodegeneration in epilepsy measured with serial MRI – Marian Galovic (Switzerland)
- Tau protein accumulation and accelerated brain ageing in chronic epilepsy – Maria Thom (United Kingdom)
- Silent seizures in Alzheimer’s disease: the interface between epilepsy and dementia – Alice Lam (USA)
Breakthroughs in focal cortical dysplasia: the ILAE classification update 2021
Co-chairs: Imad Najm (USA) & Cristina Ruedell Reschke (Ireland)
- Genetics of focal cortical dysplasia – Stéphanie Baulac (France)
- DNA methylation classifier of FCD subtypes – Katja Kobow (Germany)
- Humanized animal models of FCDs: opportunities for translational studies – Jeong Ho Lee (Korea, Republic of)
- Electroencephalographic-imaging fingerprints of FCDs – Imad Najm (USA)
Central regulation of breathing and arousal systems. An altered interplay in patients at risk of SUDEP?
Co-chairs: Sylvain Rheims (France) & Lisa Bateman (USA)
- Organisation of networks involved in central regulation of breathing and arousal systems – Sylvain Rheims (France)
- Sleep-disordered breathing in patients with epilepsy and peri-ictal respiratory Is there a relation ? – Shobi Sivathamboo (Australia)
- Impaired postictal arousal and ventilation in response to CO2: Role of serotonergic chemoreceptors – George Richerson (USA)
What’s new in epilepsy syndromes?
Co-chairs: Elaine Wirrell (USA) & Paolo Tinuper (Italy)
- Introduction: brief case presentation: ~2 year old child with SCN1A spectrum presentation – need to focus on aetiology and syndrome to choose best therapy (and possible precision therapy) – Joseph Symonds (United Kingdom)
- Genetic and idiopathic generalized epilepsy syndromes: are these terms synonymous? – Ingrid Scheffer (Australia)
- What’s new in infant/child syndromes? – Stéphane Auvin (France)
- What’s new in teen/adult/variable-aged syndromes? – Alicia Bogacz (Uruguay)
- The future: aetiology and syndrome OR aetiology-specific syndrome? – Elaine Wirrell (USA)
The microbiota gut-brain axis and epilepsy: where are we now?
Co-chairs: Astrid Nehlig (France) & Cian McCafferty (Ireland)
- Introduction to the microbiota gut-brain axis – Astrid Nehlig (France)
- The microbiota gut-brain axis: role in brain excitability and epilepsy – Emilio Russo (Italy)
- Indications for clinical practice / ketogenic diet – Heung Dong Kim (Korea, Republic of)
- Gut microbiome and post-traumatic epilepsy - Andrey Mazarati (USA)
- Microbiome and antiseizure drugs: a link for pharmacoresistance? – Patricia Lepage (France)
The rollercoaster of epilepsy genetics – what you need to know
Co-chairs: Caroline Neuray (United Kingdom) & Karl Martin Klein (Canada)
- What the clinician needs to know about genetic testing – Saskia Wortmann (Germany)
- New genes in epilepsy – phenotype-genotype correlation – Caroline Neuray (United Kingdom)
- Genetic and metabolic causes of epilepsy – where they overlap – Elaine Murphy (United Kingdom)
- Polygenic risk scores in epilepsy – Dennis Lal (USA)
What is epileptogenicity?
Co-chairs: Akio Ikeda (Japan) & Luisa Rocha (Mexico)
- Ictal and interictal DC shifts: a surrogate marker of epileptogenicity – Akio Ikeda (Japan)
- Modelling of epileptic activity by neuron and glia – Christophe Bernard (France)
- Consequences of demyelination on ictogenesia and epileptogenesis – Marco de Curtis (Italy)
- Neurological insult-induced astrocyte changes contribute to acquired epilepsy – Stefanie Robel (USA)
Can we predict the efficacy of epilepsy therapy in individual patients?
Co-chairs: Milan Brázdil (Czech Republic) & Colin Josephson (Canada)
- AI meets drug treatment, the future begins now – Margitta Seeck (Switzerland)
- The virtual brain predicting epilepsy surgery outcomes and protecting brains – Viktor Jirsa (France)
- Prediction of individual neurostimulation efficacy in intractable epilepsy – dreams or reality? – Milan Brázdil (Czech Republic)
- From ‘trial and error’ to personalised care of epilepsies – Patrick Kwan (Australia)
The new era of implantable EEG
Co-chairs: Troels Wesenberg Kjær (Denmark) & Margitta Seeck (Switzerland)
- Subcutaneous EEG in ultra-long-term seizure monitoring – Troels Wesenberg Kjær (Denmark)
- The “fit-bit” for the brain forecasts seizures – Mark Cook (Australia)
- Chronic EEG: bringing research and clinic together – Maxime Baud (Switzerland)
- Under reporting and over reporting of seizures – Gregory Worrell (USA)
MRI-negative epilepsy: myth or reality with current techniques?
Co-chairs: Irene Wang (USA) & Aileen McGonigal (France)
- Making the invisible visible: the yield of structural MRI – Neda Ladbon-Bernasconi (Canada)
- Localisation yield of SEEG and seizure outcome in MRI-negative epilepsy – Aileen McGonigal (France)
- Functional MRI and connectivity analysis in non-lesional epilepsy – Graeme Jackson (Australia)
Psychiatric issues in paediatric epilepsy
Co-chairs: Kette Valente (Brazil) & Sharon Whiting (Canada)
- ADHD and epilepsy: the ILAE consensus on screening, diagnosis, and treatment – Kirsty Donald (South Africa)
- A proactive behavioural medicine approach – Kette Valente (Brazil)
- Aggressive behaviour in adolescents with ID/ASD and epilepsy: When seizure control is not the main complaint – Michael Kerr (United Kingdom)
Opportunities and challenges in the delivery of care
Co-chairs: William Theodore (USA) & Amza Ali (Jamaica)
- The role of technology in closing the treatment gap – Amza Ali (Jamaica)
- Epilepsy care in China: a clinic of 3 billion people – Shichuo Li (China)
- A primary healthcare model to reduce the epilepsy treatment gap – Palmira Fortunato dos Santos (Mozambique)
- Interventions to improve access to epilepsy care: is there any evidence of effectiveness? – Archana Patel (USA)
Genetics, drug discovery and stigma in the ILAE years
Co-chairs: Simon Shorvon (United Kingdom) & Ingrid Scheffer (Australia)
- Genetics and epilepsy over time – Howard Goodkin (USA)
- The development of the concepts of drug discovery – Meir Bialer (Israel)
- How stigma has changed – the image of epilepsy in literature – Peter Wolf (Denmark)
Post traumatic epilepsy
Co-chairs: Pablo Casillas-Espinosa (Australia) & Aristea Galanopoulou (USA)
- Introduction: the challenge and promise of epilepsy therapy development – Terence O’Brien (Australia)
- Pre-clinical biomarkers of epileptogenesis – Asla Pitkänen (Finland)
- Trials of antiepileptogenic therapies: what works? what doesn’t? – Aristea Galanopoulou (USA)
- Modifying epilepsy once it occurs: can we reverse the progression of epilepsy and its associated comorbidities? – Pablo Casillas-Espinosa (Australia)
- Post-traumatic epilepsy after TBI: psychosocial elements, risk factors, how it develops and complicates recovery after TBI – tbc
Multifaceted aspects of sleep and epilepsy
Co-chairs: Birgit Frauscher (Canada) & Sofia Eriksson (United Kingdom)
- Sleep improves identification of the epileptogenic zone – Birgit Frauscher (Canada)
- Anatomo-electroclinical features of sleep related hypermotor seizures and parasomnias – Lino Nobili (Italy)
- Genetics of sleep related epilepsies – Stéphanie Baulac (France)
- Specific management of sleep-related epilepsies – Sofia Eriksson (United Kingdom)
Looking into the causes of psychogenic nonepileptic seizures: the contribution of imaging studies
Co-chairs: Markus Reuber (United Kingdom) & Kette Valente (Brazil)
- Short introduction: What imaging studies need to explain: an integrative aetiological model of PNES – Markus Reuber (United Kingdom)
- PNES-associated network changes and their significance – Selma Aybek (Switzerland)
- PNES and brain developing – insights from studies of young brains? – Kasia Kozlowska (Australia)
- PNES: a problem with hardware or software? – Jerzy Szaflarski (USA)
Towards precision medicine in cortical malformations
Co-chairs: Jean-Bernard Manent (France) & Iscia Lopes-Cendes (Brazil)
- On the way towards AI-based decision support systems – Samir Jabari (Germany)
- Mechanisms of mTOR-induced epilepsy – Lena Nguyen (USA)
- Novel genetic screening techniques in cortical malformations – Jin-Wu Tsai (Taiwan, Rep of China)
- Epileptogenic networks in cortical malformations – Jean-Bernard Manent (France)
Management of autoimmune epilepsy in the era of biomarkers
Co-chairs: Divyanshu Dubey (USA) & Sarosh Irani (United Kingdom)
- Antibody biomarkers of acute symptomatic seizures secondary to autoimmune encephalitis and autoimmune epilepsy – Divyanshu Dubey (USA)
- Utility of cytokine and chemokine profiles in the diagnosis and management of autoimmune and auto-inflammatory epilepsies – Eric Payne (Canada)
- Acute and chronic management of autoimmune syndromes associated epilepsy guided by biomarkers – Khalil Husari (USA)
Post-stroke epilepsy – Predict! Protect. Prevent?
Co-chairs: Alla Guekht (Russian Federation) & Marian Galovic (Switzerland)
- Prediction tools for post-stroke epilepsy – Carla Bentes (Portugal)
- AEDs and stroke prevention drugs: preferences and pitfalls – Alla Guekht (Russian Federation)
- Epileptogenesis in PSE? – Asla Pitkänen (Finland)
- Epileptogenicity after stroke – any chance to protect? – Eugen Trinka (Austria)
Sex matters – reproductive health in epilepsy
Co-chair: Oliver Henning (Norway) & Katia Lin (Brazil)
- Sexual dysfunction in persons with epilepsy – Oliver Henning (Norway)
- Treatment of sexual dysfunction – Gerhard Luef (Austria)
- Pregnancy and motherhood in epilepsy – Page Pennell (USA)
- Relationships and seizure control – Sarah Wilson (Australia)
Suicide and seizures – management in routine clinical care
Co-chairs: Rosa Michaelis (Germany) & Natela Okujava (Georgia)
- Suicide and ideation in patient with epilepsy: epidemiology and overview – Rosa Michaelis (Germany)
- ILAE surveys: suicidality screening, mental health screening and management practices throughout the world – Milena Gandy (Australia)
- Examples and tips for best practice: How to talk about suicide in a busy epilepsy clinic – adults – Marco Mula (United Kingdom)
- Recognising suicidal ideation in paediatric patients: working with patients and families – Avani Modi (USA) & Janelle Wagner (USA) (with additional input by Kirsty Donald (South Africa))
Status epilepticus – new concepts and novel therapies (part 1)
Chair: Eugen Trinka (Austria)
- Molecular and cellular mechanism in status epilepticus – Karen Wilcox (USA)
- Uncommon and rare causes of status epilepticus – Nicolas Gaspard (Belgium)
Status epilepticus – new concepts and novel therapies (part 2)
Chair: Eugen Trinka (Austria)
- Neuroimaging of status epilepticus – making the invisible visible – Pilar Bosque-Varela (Austria)
- Novel treatments for refractory and super refractory status epilepticus – Matthew Walker (United Kingdom)
Neonatal update
Co-chairs: Ronit Pressler (United Kingdom) & Perrine Plouin (France)
- Classification of seizures and epilepsy syndromes in neonates – Ronit Pressler (United Kingdom)
- Genetics of neonatal onset epilepsy syndromes – Sarah Weckhuysen (Belgium)
- Treatment of neonatal seizures revisited – Jo Wilmshurst (South Africa)
Neurobiology Symposium: Neurobiology of SARS-CoV-2 / COVID-19 and relevance to epilepsy
Chair: Aristea Galanopoulou (USA)
- Presentation of Harinarayan Awards to Gabriele Lignani (United Kingdom) and Hyunyong Koh (USA)
- Neurobiology and neuroinvasion of SARS-CoV-2 – Eric Song (USA)
- Neuropathology and inflammatory response in COVID-19 – Marianna Bugiani (Netherlands)
- Coagulation, neurovascular unit, blood brain barrier: breaking down a link between COVID-19 and seizures?
- COVID-19 and seizures: is there a link? – Victor Ferastraoaru (USA)
Gene therapy for pharmacoresistant epilepsy – principles, opportunities, and pitfalls
Co-chairs: Simona Balestrini (United Kingdom) & Premysl Jiruska (Czech Republic)
- Pharmacoresistant epilepsy – neurobiological substrates for gene therapy – Merab Kokaia (Sweden)
- Does gene therapy work? Principles and experience from animal studies – Stephanie Schorge (United Kingdom)
- Gene therapy for epilepsy in humans – promises and pitfalls – Renzo Guerrini (Italy)
Refractory early-life seizures: taking evidence-based insights from basic science into the hands of clinicians
Co-chairs: Shilpa Kadam (USA) & Ronit Pressler (United Kingdom)
- Bumetanide analogues for the treatment of refractory neonatal seizures: past, present and future – Wolfgang Löscher (Germany)
- The challenges of detecting seizure in neonates in NICU which by default makes it hard to optimise treatment protocols – Geraldine Boylan (Ireland)
- Small molecules that restore GABA as a therapeutic target to treat Autism Spectrum Disorder – James Clement (India)
Epigenetics and epilepsy collide: unravelling mechanisms, treatments and diagnostics
Chair: David Henshall (Ireland)
- (Post)transcriptional profiling in human epilepsy – Albert Becker (Germany)
- Chromatin landscape of human temporal lobe epilepsy – Karen Conboy (Ireland)
- Small non-coding RNAs as novel therapeutic targets and biomarkers for epilepsy – Erwin van Vliet (Netherlands)
Workshop: Clinical Practice Guideline (CPG) development and implementation
Co-chairs: Nathalie Jette (USA) & Francesco Brigo (Italy)
- Welcoming remarks – Nathalie Jette (USA)
- Introduction: what is a CPG and what are alternative methods when the evidence is limited?
- What is and what is not a guideline? – Katia Lin (Brazil)
- When a CPG is not feasible: consensus recommendations including Delphi method (will include real example from an ILAE commission) – Nathalie Jette – (USA)
- How to develop a CPG
- From formulating the clinical question to making final recommendations – Francesco Brigo (Italy)
- ILAE neonatal seizures guidelines – a real life example – Ronit Pressler (United Kingdom) & Hans Hartmann (Germany)
- How to implement a CPG in different settings: the ADAPTE Process and how to implement CPG – Marco Mula (United Kingdom)
- Concluding remarks – Francesco Brigo (Italy)
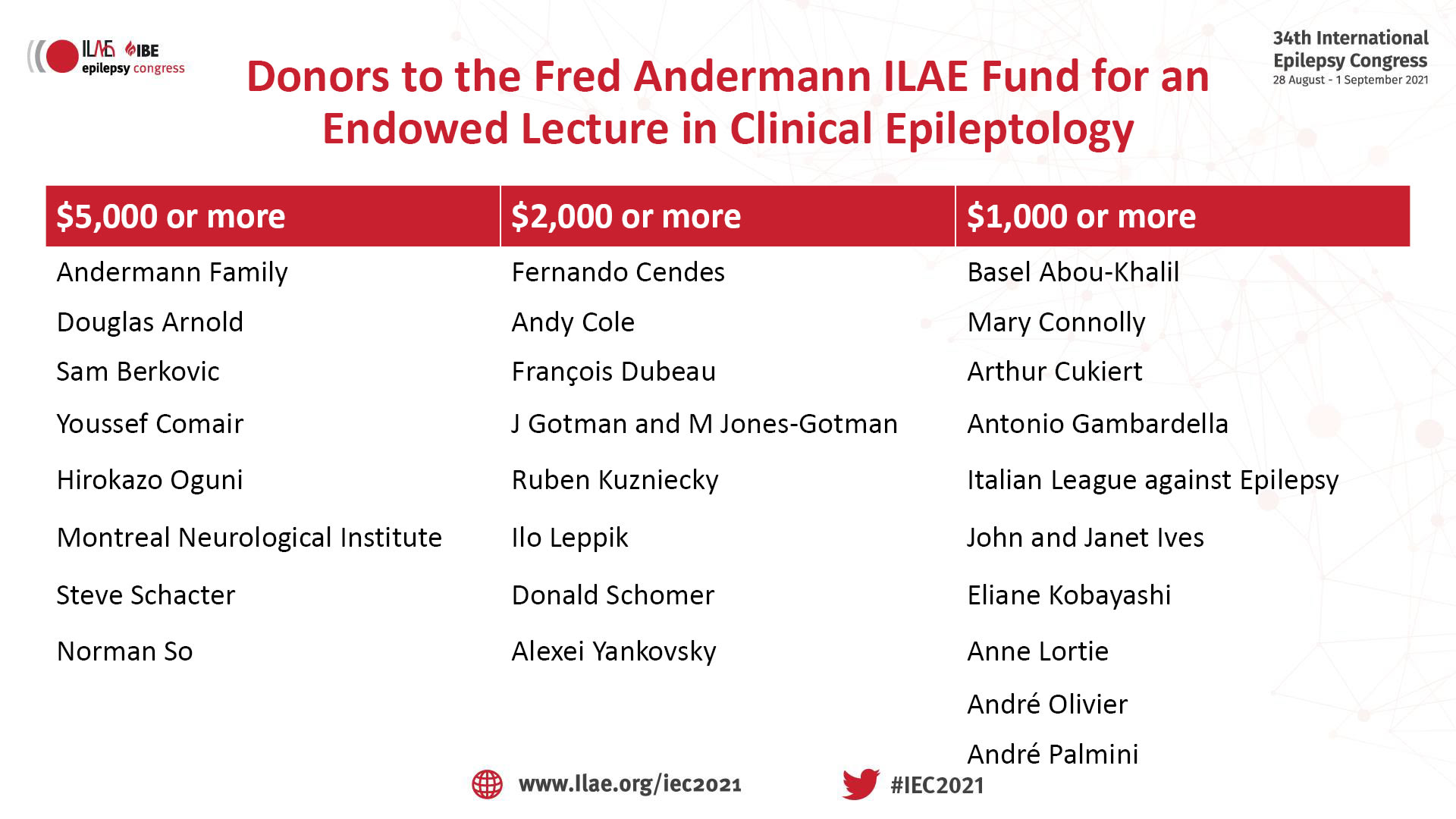
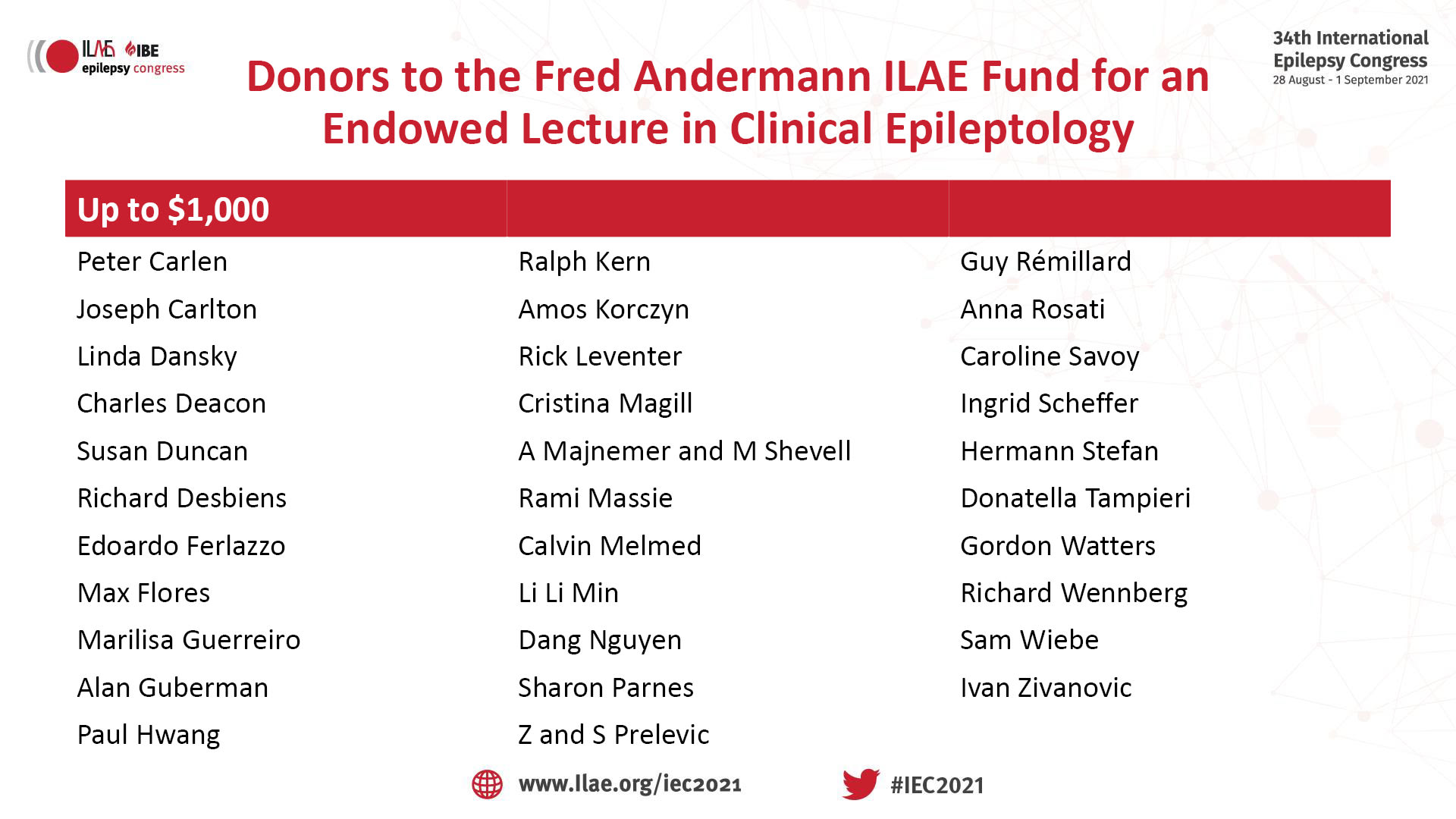
ILAE - Fred Andermann Lecture in Clinical Epileptology
Co-chairs: Samuel Wiebe (Canada) & J Helen Cross (United Kingdom)
- Some words about Fred Andermann - François Dubeau (Canada)
- Does epilepsy still exist?: the changing concepts of epilepsy in the last 150 years - Simon Shorvon (United Kingdom)
Debate: Do we need to record seizures to know where they are coming from?
Moderator: Maeike Zijlmans (Netherlands)
- It is critical to record the seizure onset to ensure surgical success – Philippe Kahane (France)
- It is not possible to be sure that the seizure onset has been recorded and we do not need to know – Jean Gotman (Canada)
Controversies in epilepsy: are ASMs disease-modifying or not?
Chair: Sanaz Ahmadi Karvigh (Iran)
- Yes – Jacqueline French (USA)
- No – Emilio Perucca (Italy)
Controversies in epilepsy: is it autoimmune encephalitis with seizures or is it autoimmune epilepsy?
Chair: Christian Bien (Germany)
- Jeffrey Britton (USA)
- Sarosh Irani (United Kingdom)
Both sides of the coin: considering behavioural disorders when managing epilepsy and vice versa
Moderators: Kette Valente (Brazil), Stéphane Auvin (France), Michael Kerr (United Kingdom)
- A boy with typical absence syndrome with total remission after treatment that presents with academic issues and evolves with school refusal – Elaine Wirrell (USA) & Stéphane Auvin (France)
- A 5-year-old child with Dravet syndrome and SCN1A mutation, diagnosed with autism that evolves with aggressive behaviour – Jo Wilmshurst (South Africa) & Jay Salpekar (USA)
- A 15-year-old girl with JME showing low-adherence to treatment. During follow-up, the family reports marijuana use and mood swings – Mary Lou Smith (Canada) & Marco Mula (United Kingdom)
Surgical evaluation
Chair: Laura Tassi (Italy)
- Extra temporal case – Lara Jehi (USA)
- Lesional case – Laura Tassi (Italy)
- Extra temporal non lesional case – Francesca Pizzo (France)
Using antiseizure medicines optimally. YES or no?
Co-chairs: Martin Brodie (Scotland) & Emilio Perucca (Italy)
- What treatment and what doses? Risk and benefits of antiseizure medication in a young woman with refractory epilepsy secondary to bilateral periventricular nodular heterotopia (PVNH) – Simona Balestrini (United Kingdom)
- Antiseizure medications and novel oral anticoagulants: should we optimize neurological, or cardiological drugs or both? – Margherita Contento (Italy)
- Starting treatment in a patient with a diagnosis of seizure disorder associated with MS – Anca Arbune (Romania)
- Epilepsy and forced normalization: optimizing management – Fabrizio Rinaldi (Italy)
- A challenging case of idiosyncratic adverse reactions to multiple antiseizure medications – Lili Long (China)
- Successful management of an infant with drug resistant epilepsy – Sebastián Ortiz De la Rosa (Colombia)
Full-Day Teaching Course: Neuroimaging in epilepsy – what the clinician should know
Chair: Paolo Federico (Canada)
- Introduction to neuroimaging in epilepsy – Paolo Federico (Canada)
- MRI physics, sequence names, and MRI epilepsy protocol – Boris Bernhardt (Canada)
- Common epileptic pathologies: temporal epilepsy – Neda Labdon-Bernasconi (Canada)
- Common epileptic pathologies: extratemporal lobe epilepsy – Fernando Cendes (Brazil)
- Hands-on session – Paolo Federico (Canada), Boris Bernhardt (Canada), Neda Labdon-Bernasconi (Canada), Fernando Cendes (Brazil), Andrea Bernasconi (Canada), Yotin Chinavarun (Thailand), Anna Elisabetta Vaudano (Italy), Graeme Jackson (Australia), Lorenzo Caciagli (USA), Luis Concha (Mexico), Victoria Morgan (USA), Irene Wang (USA), Shuang Wang (China), Stefan Rampp (Germany)
- MRI-negative epilepsy. What are the next steps? – Andrea Bernasconi (Canada)
- Other neuroimaging modalities: PET, SPECT – Yotin Chinavarun (Thailand)
- fMRI (task-based) and EEG-fMRI – Anna Elisabetta Vaudano (Italy) & Graeme Jackson (Australia)
- Hands-on session – Paolo Federico (Canada), Boris Bernhardt (Canada), Neda Labdon-Bernasconi (Canada), Fernando Cendes (Brazil), Andrea Bernasconi (Canada), Yotin Chinavarun (Thailand), Anna Elisabetta Vaudano (Italy), Graeme Jackson (Australia), Lorenzo Caciagli (USA), Luis Concha (Mexico), Victoria Morgan (USA), Irene Wang (USA), Shuang Wang (China), Stefan Rampp (Germany)
- Group discussion/feedback – Paolo Federico (Canada), Boris Bernhardt (Canada), Neda Labdon-Bernasconi (Canada), Fernando Cendes (Brazil), Andrea Bernasconi (Canada), Yotin Chinavarun (Thailand), Anna Elisabetta Vaudano (Italy), Graeme Jackson (Australia), Lorenzo Caciagli (USA), Luis Concha (Mexico), Victoria Morgan (USA), Irene Wang (USA), Shuang Wang (China), Stefan Rampp (Germany)
Half-Day Teaching Course: EEG in diagnosing patients with epilepsy (EEG starter)
Co-chairs: Sándor Beniczky (Denmark) & Donald Schomer (USA)
- Basic technology, electrodes, montages and localisation- Donald Schomer (USA)
- Systematic approach to EEG interpretation: background activity – William Tatum (USA)
- Normal variants. Sensitivity and specificity – Selim Benbadis (USA)
- Systematic approach to EEG interpretation: interictal and ictal patterns – Sándor Beniczky (Denmark)
Half-Day Teaching Course: Epilepsy diagnosis
Co-chairs: Peter Wolf (Denmark) & Walter van Emde Boas (Netherlands)
- Is this seizure? Recognizing and classifying seizures from patient history and from video recordings – Peter Wolf (Denmark) & Walter van Emde Boas (Netherlands)
- Localizing focal seizures based on patient history and video recordings – Philippe Kahane (France)
- Aetiologies according to the age of onset – Michael Sperling (USA)
- Epilepsy syndromes – Tiziana Granata (Italy)
Half-Day Teaching Course: Pharmacological treatment: starter course
Co-chairs: Emilio Perucca (Italy) & Torbjörn Tomson (Sweden)
- Basic and clinical pharmacology – Matthew Walker (United Kingdom)
- Drug treatment: When to start and when to stop – Terence O’Brien (Australia)
- Drug selection and titration – Emilio Perucca (Italy)
- Special populations: women and elderly – Torbjörn Tomson (Sweden)
- Special populations: infants and children – Elaine Wirrell (USA)
Half-Day Teaching Course: Status epilepticus
Chair: Eugen Trinka (Austria)
- Epidemiology and classification – Eugen Trinka (Austria)
- Pathophysiology and consequences of status epilepticus – Karen Wilcox (USA)
- Diagnosis and treatment: part one – Matthew Walker (United Kingdom)
- Diagnosis and treatment: part two – Nicolas Gaspard (Belgium)
Teaching Course: EEG source imaging virtual workshop
- Stefan Rampp (Germany)
- Sándor Beniczky (Denmark)
Teaching Session: Counselling patients with epilepsy, caregivers and relatives
- Martin Brodie (Scotland)
- Mary Secco (Canada)
Teaching Session: Developmental and epileptic encephalopathies
- Developmental and epileptic encephalopathy: definition and pathophysiology – Ingrid Scheffer (Australia)
- Genetic and metabolic investigation: the impact for patients care – Rima Nabbout (France)
- Treatment of epileptic encephalopathy – J Helen Cross (United Kingdom)
Teaching Session: VIREPA courses: EEG (basic and advanced)
- VIREPA courses: Basic EEG – Elena Gardella (Denmark)
- VIREPA courses: Advanced EEG – Antonio Valentin (United Kingdom)
Teaching Session: VIREPA courses: Sleep and paediatric EEG
- VIREPA courses: Paediatric EEG – Monika Eisermann (France)
Teaching Session: Video session: is this epilepsy or not?
- Children – Jo Wilmshurst (South Africa)
- Adults – Ivan Rektor (Czech Republic)
Teaching Session: Video session: focal seizures
- Philippe Kahane (France)
- Philippe Ryvlin (Switzerland)
Teaching Session: Video session: generalised seizures
- Ronit Pressler (United Kingdom)
- Guido Rubboli (Denmark)
Award Symposium: Michael Prize
Chair: Bettina Schmitz (Germany)
- Towards DNA methylation-based disease classification in focal epilepsy – Katja Kobow (Germany)
Award Symposium: ‘Epilepsia’ Prize – Basic Science
Co-chairs: Astrid Nehlig (France) & Michael Sperling (USA)
- Progressive cardiorespiratory dysfunction in Kv1.1 knockout mice may provide temporal biomarkers of pending sudden unexpected death in epilepsy (SUDEP): The contribution of orexin – Shruthi Iyer (USA)
Award Symposium: ‘Epilepsia’ Prize – Clinical Science
Co-chairs: Astrid Nehlig (France) & Michael Sperling (USA)
- Machine learning from wristband sensor data for wearable, noninvasive seizure forecasting – Christian Meisel (Germany)
Award Symposium: ‘Epilepsia Open’ Prize – Basic Science
Chair: Aristea Galanopoulou (USA)
- COX‐2/PGE2 axis regulates hippocampal BDNF/TrkB signaling via EP2 receptor after prolonged seizures – Ying Yu (USA)
Award Symposium: ‘Epilepsia Open’ Prize – Clinical Science
Chair: Aristea Galanopoulou (USA)
- Impact of diagnostic delay on seizure outcome in newly diagnosed focal epilepsy – Laura Parviainen (Finland)
Award Symposium: ‘Epileptic Disorders’ Educational Prize
Chair: Sándor Beniczky (Denmark)
- Characterizing Sunflower syndrome: a clinical series – James Barnett (USA)
The ILAE Commission on Surgical Therapies is organising a 1-day symposium on Wednesday 1 September, between 09.30 and 16.30 UTC+1. The overall theme will be “Planning for success in epilepsy surgery”.
Major advances have occurred over the past decade in the context of both pre-surgical evaluations and surgical techniques. On the diagnostic end, structural and functional imaging have evolved to allow exponential improvements in the localization of drug-resistant focal epilepsy. On the therapeutic end, invasive EEG modalities such as stereo EEG have become more accessible, increasing the pool of patients who could undergo these complex procedures. Minimally invasive surgical options such as Laser Interstitial Thermal Therapy and focused ultrasound are offering additional treatment options beyond resective epilepsy surgery.
In conjunction with this evolving diagnostic and procedural landscape, there is a growing appreciation of the need to expand our definition of success in epilepsy surgery beyond a reductionist approach limited to complete seizure freedom. Favourable neuropsychological outcomes, improved overall quality of life, and significant seizure palliation, are all major patient goals that need to be considered in surgical planning.
In this symposium, we will review highlights of major advancements in both diagnostic and surgical techniques, and discuss more comprehensive approaches to outcomes assessment. This goal will be accomplished through a series of didactic lectures, interspersed with neurosurgical training videos, and discussions of controversial subjects. Opportunities for questions and answers sessions will be available.
The following ILAE Educational Curriculum Competencies will be addressed:
4.3: Demonstrate working knowledge of advanced techniques for presurgical evaluation.
4.5: Demonstrate ability to integrate information from multi-modal work-up and estimates risks and benefits of surgical therapy.
Introduction
- Relevance of planning and measuring success in epilepsy surgery – Lara Jehi (USA)
Session 1: Advances in imaging
- Imaging epileptic networks – Fabrice Bartolomei (France)
- Structural MRI: from eyeballing to fingerprinting – Fernando Cendes (Brazil)
- Imaging integration in the OR – Karl Roessler (Austria)
- Q&A
Session 2: Advances in surgical techniques
- LITT – Robert Gross (USA)
- Focused ultrasound – Ellen Bubrick (USA)
- Subdural electrodes, stereo EEG, both, or neither? – Kees Braun (Netherlands)
- Q&A
Session 3: Balancing seizure freedom with “everything else”
- Stating the problem – Dario Englot (USA)
- Innovating in outcome measurement – Samuel Wiebe (Canada)
- Neuropsychological outcomes with minimally ablative and resective surgery – Sallie Baxendale (United Kingdom)
- Seizure freedom, extent, and timing of resection – J Helen Cross (United Kingdom)
- Q&A
Session 4: Controversial topics and future direction
- Interneuron transplantations for epilepsy: basic science and potential for human trials – Derek Southwell (USA)
- The latest in brain stimulation for epilepsy – Kristl Vonck (Belgium)
- Is all this technology worth it? – Robert Fisher (USA)
- Q&A
Closing remarks
- Lara Jehi (USA)
Kindling epileptogenesis: beginnings and future
Epilepsy research has achieved remarkable progress through the years, evolving in concepts, models, techniques and approaches. While the younger generation is familiar with these tools and concepts, they are less familiar with the pioneers who conducted these studies or the history behind these ground-breaking discoveries that pushed the field forward. The overall goal of this session is to merge history and future and discuss how past experiences may help shape and inform the future of epilepsy research but also serve as guidance for the younger investigator as they strive to develop their research careers.
The session will include brief video recordings of research neuroscience pioneers, many of whom played a critical role in forming the neurobiology research strategies and initiatives of the ILAE across the years, discussing their early scientific discoveries in the context of the times these were developed. Pre-recorded interviews with Gyorgy Buzsaki, Jerome (Pete) Engel Jr, Claude Wasterlain, Solomon (Nico) Moshé, Giuliano Avanzini, Astrid Nehlig, Anamaria Vezzani will be presented, revisiting some of the old breakthrough studies on brain rhythms, kindling experiments, networks, systems epilepsy and big data analyses.
In parallel, a panel of younger scientists will present brief presentations of their current research followed by discussion. The session is expected to relate to a wider audience of neuroscientists and epileptologists at various career stages and will provide an opportunity to discuss the future of epilepsy research under the light of past and current achievements.
Co-chairs: Aristea Galanopoulou (USA) & David Henshall (Ireland)
- Welcome - Aristea Galanopoulou (USA) & David Henshall (Ireland)
- Interview with Gyorgy Buzsaki (USA)
- Interview with Jerome (Pete) Engel Jr (USA)
- Interictal epileptiform discharges shape large scale intercortical communications - Jennifer Gelinas (USA)
- Rhythmopathies, microcircuits and epilepsy - Liset Menendez de la Prida (Spain)
- Q&A
- Interview with Claude Wasterlain (USA)
- Interview with Solomon (Nico) Moshé (USA)
- HippoBellum. Cerebellum and epilepsy - Esther Krook-Magnuson (USA)
- Cortical-subcortical networks in the control of seizures - Patrick Forcelli (USA)
- Q&A
- Interview with Giuliano Avanzini (Italy)
- Interview with Astrid Nehlig (France)
- Interview with Annamaria Vezzani (Italy)
- Epilepsy crossroads: beyond neurons and epilepsy networks - Melissa Barker-Haliski (USA)
- Genetic epilepsies and precision medicine - Stephanie Schorge (United Kingdom)
- The ENIGMA-Epilepsy: mapping disease from large data sets - Sanjay Sisodiya (United Kingdom)
IBE Day at the 34th International Epilepsy Congress
The IBE Day is taking place on Wednesday 1 September as part of the IEC. It consists of 3 two-hour virtual sessions on topical issues that affect the day-to-day lives of people living with epilepsy.
This virtual event will cover topics including making epilepsy a national health priority – intersectoral collaboration, empowering youth to raise their voices and best practices to address the psychosocial impact of epilepsy.
Additionally, the IBE International Golden Light Awards will be presented; the IBE Golden Light Awards recognise the contributions of people affected by epilepsy in their community and those who care for them.
We hope that the virtual experience allows more people around the globe to participate in the IBE Day. Access to these sessions is free of charge for IBE chapters and their members, but registration is necessary.
REGISTER FOR IBE DAY
The programme for the IBE Day may be downloaded here.
Making epilepsy a national health priority – intersectoral collaboration
Co-chairs: Mary Secco, IBE Secretary General (Canada) & Action Amos, IBE Vice President Africa (Malawi)
- 10-year intersectoral global action plan on epilepsy and other neurological disorders (IGAP) – Tarun Dua, WHO Brain Health Unit (Switzerland)
- Improving care for children with neurological disorders in resource poor settings – Jo Wilmshurst, President International Childhood Neurology Association (South Africa)
- Improving access to essential medicines – Gaby Ooms, Health Action International (Netherlands)
- Putting epilepsy on social policy and development agendas [tbc] – John O’Toole, Division for Inclusive Social Development (DISD), UN Department of Economic and Social Affairs (USA)
- Leveraging the IGAP to improve care for people with epilepsy – Alla Guekht, Chair ILAE Global Advocacy Council (Russian Federation)
- Working with donors – Gardiner Lapham, Trustee BAND Foundation (USA)
- Epilepsy advocate’s toolkit – Karen Robinson, Epilepsy South Africa (South Africa)
- Global Health in Epilepsy Database – Karen Parko, ILAE North America (USA)
Empowering youth to raise their voices
Co-chairs: Lorraine Lally (Ireland) & Scarlett Paige (Australia), co-chairs of the IBE Youth Team
- Epilepsy & Pregnancy: launching IBE’s new toolkit – Lorraine Lally (Ireland) & Gus Baker, Chair Epilepsy & Pregnancy Campaign and IBE Secretary General-elect (United Kingdom)
- Meet the International Golden Light Award Winners 2021
- Presentation of 19 awardees
- Hear my Story
- International Golden Lights, from IBE’s seven regions, share their personal stories:
- Africa: Bright Bwalya (Zambia)
- Eastern Mediterranean: Mohsen Fariborzi (Iran)
- Europe: Lynna Held (Germany)
- Latin America: Luiza Gatto (Brazil) & Valentina Kahn (Chile)
- North America: Cassidy Megan (Canada)
- South East Asia: Vinay Jani (India)
- Western Pacific: Meng-Leo Chou (Taiwan China)
- Introduction to the IBE Global Youth Team – Lorraine Lally (Ireland) & Scarlett Paige (Australia)
- Questions and Answers session
Psychologic treatment and self-management of epilepsy
Chair: Gus Baker, IBE Secretary General-elect (United Kingdom)
- The comorbidities of epilepsy: a review – Gus Baker, Chair IBE Research Team and Secretary-General-elect (United Kingdom)
- The psychological management of epilepsy: the Turkish experience – Nuran Aydemir, Co-chair IBE Research Team (Turkey)
- Self-management programmes in children: the Scottish experience – Liam Dorris (Scotland)
- Psychological treatment of epilepsy: the Mauritius experience – Devishada Dassyne (Mauritius)
- Self-management programmes: the US experience – Rosemarie Kobau (USA)
For any general queries on the IBE Day, please contact the Congress Secretariat at iec@epilepsycongress.org.
ILAE YES Career Development Session: Effective scientific communication: from securing funding to engaging the public
Chair: Pablo Casillas-Espinosa (Australia)
- Effective scientific communication: from securing funding to engaging the public - Jackie Ashley (United Kingdom)
ILAE YES Career Development Session: New skill, upskill or re-skill? Transitioning to alternative career paths
Chair: Cristina Ruedell Reschke (Ireland)
- Academia vs industry: a testimony of a dual career path - Stefanie Dedeurwaerdere (Belgium)
- My road to CURE epilepsy - Laura Lubbers (USA)
ILAE YES Career Development Session: How To session
Chair: Diego Jiménez Jiménez (United Kingdom)
- Revising it right: how to get that paper to the end of the line - Dimitri Kullmann (United Kingdom)
ILAE YES Brainstorming Session: NORSE: New Onset Refractory Status Epilepticus
Moderator: Ruta Yardi (USA)
- NORSE: New Onset Refractory Status Epilepticus - Nicolas Gaspard (Belgium)
ILAE YES Brainstorming Session: Choosing a first line antiseizure medication: the SANAD studies in context
Moderator: Mirja Steinbrenner (Germany)
- Choosing a first line antiseizure medication: The SANAD studies in context - Anthony Marson (United Kingdom)
ILAE YES Brainstorming Session: Real-time EEG analysis and closed-loop of seizures
Moderator: Christos Lisgaras (USA)
- Real-time EEG analysis and closed-loop of seizures - Esther Krook-Magnuson (USA)
Adult epileptology
Chair: Fatema Abdulla (Bahrain)
399 Factors influencing the daily evolution of preictal connectivity dynamics in epilepsy – Jakub Kopal (Czech Republic)
430 Cardiac autonomic response to hyperventilation and risk of SUDEP – William Szurhaj (France)
243 Spectral shifts across distributed networks in cortex predict seizure onset – Maryam Hasanzadeh Mofrad (Canada)
468 Juvenile myoclonic epilepsy: Outcome beyond three decades from onset- A hospital based cohort study – Harini Pavuluri (India)
Basic sciences
Chair: Christina Ruedell Reschke (Ireland)
882 Activity-dependent Gene Therapy for Intractable Epilepsy – Gabriele Lignani (United Kingdom)
260 Non-cell autonomous hyperexcitability underlies focal epileptogenesis mediated by low-level brain somatic mutations in MTOR – Hyunyong Koh (USA)
455 Robust chronic convulsive seizures, high-frequency oscillations, and human seizure onset patterns in an intrahippocampal kainic acid model in mice – Christos Lisgaras (USA)
801 Adenovirus-mediated expression of NaV1.1 ameliorates Dravet syndrome epilepsy in mice – Saja Fadila (Israel)
Clinical neurophysiology
Chair: Jorge Burneo (Canada)
587 Fully-Automated Spike Detection and Dipole Analysis of Epileptic Magnetoencephalograms Using Deep Learning – Masayuki Hirata (Japan)
627 Seizure-onset EEG patterns in malformations of cortical development: a systematic review – Lubna Shakhatreh (Australia)
695 Surgery-Related Changes in Sleep Spindle Activity of Children with Drug-Resistant Epilepsy – Assia Chericoni (USA)
368 Artificial Intelligence outperforms Quantitative EEG Assessment for Seizure Detection of ICU Patients – Franz Fürbass (Austria)
Drug therapy
Chair: Sanjeev Thomas (India)
555 Machine learning based prediction model for initial antiseizure medication selection in newly diagnosed epilepsy – Haris Hakeem (Australia)
1204 Comparison of the effects of new anti-seizure drugs (ASDs) on cardiac autonomic control in patients with temporal lobe epilepsy (TLE) – Fedele Dono (Italy)
141 Time to Onset of Cannabidiol Treatment Effect and Resolution of Adverse Events in Tuberous Sclerosis Complex Randomised Controlled Trial (GWPCARE6) – Rocio Sanchez-Carpintero (Spain)
689 Cerliponase alfa for treatment of CLN2 disease in a patient cohort including children
Epidemiology
Chair: Churl-Su Kwon (USA)
643 Incidence, severity and outcomes of COVID-19 in elderly people with epilepsy in Moscow: case-control study – Flora Rider (Russian Federation)
185 The Global Economic Burden of Epilepsy – Charles Begley (USA)
303 Prenatal exposure to antiseizure medication and intrauterine growth restriction in offspring of women with epilepsy – Julie Dreier (Denmark)
711 Adult-onset epilepsy is defined by phenotypic clusters with unique comorbidities and risks of death – Colin Josephson (Canada)
Epilepsy in special groups
Chair: Martin Brodie (Scotland)
272 Point-of-care EEG-video in northern Nigeria emergency rooms (ERs) utilizing community healthcare workers (CHWs) trained in EEG technology – Umar Sabo (Nigeria)
421 Using health laws to prioritise epilepsy in resource-restricted settings: an African perspective – Nkandu Nchindila (South Africa)
665 Bridging the Childhood Epilepsy Treatment Gap in Africa (BRIDGE): A Cluster Randomized Clinical Trial of Task-Shifted Epilepsy Care – Aminu Taura (Nigeria)
773 Prenatal exposure to antiseizure medication duotherapy and risk of neurodevelopmental disorders – SCAN–AED: a Nordic nationwide cohort study – Marte Helene Bjork (Norway)
Epilepsy surgery
Chair: Bertil Rydenhag (Sweden)
190 Combining Intracranial EEG Measures of Brain Connectivity and Excitability to Plan Epilepsy Surgery in Children – Eleonora Tamilia (USA)
650 Prognostic model for withdrawal of anti-seizure medications following epilepsy surgery in adults: a worldwide multicentre study – Carolina Ferreira-Atuesta (United Kingdom)
745 Paediatric epilepsy surgery from 2000 to 2018: have we reached a plateau in seizure freedom rates? – Maria Eriksson (United Kingdom)
444 Comparison of the real-world effectiveness of vertical versus lateral functional hemispherotomy techniques for pediatric drug-resistant epilepsy – Alexander Weil (Canada)
Genetics
Chair: Katja Kobow (Germany)
515 Everolimus as a precision therapy for drug-resistant epilepsy caused by mutations in the GATOR1 complex genes DEPDC5 and NPLR3 – Patrick B. Moloney (Ireland)
972 Genetic Landscape of Infantile Spasms with Focal Brain Malformations – Matthew Coleman (Australia)
080 Genotype-phenotype correlations in SCN8A-related disorders reveal prognostic and therapeutic implications – Katrine Marie Johannesen (Denmark)
653 Functional assessment of KCNB1 loss- and gain-of-function variants and correlation with electro-clinical phenotypes – Antonella Riva (Italy)
Neuroimaging
Chair: Anna Elisabetta Vaudano (Italy)
577 Structural covariance network changes in the common epilepsies: a worldwide ENIGMA study – Sara Larivière (Canada)
828 MELD Project: Predictors of lesion location and postsurgical seizure freedom in focal cortical dysplasia (FCD) – Sophie Adler (United Kingdom)
178 Focal hypertrophy in mesial temporal lobe epilepsy – Richard Zubal (Switzerland)
237 Extent of resection and optimal postsurgical memory and seizure outcome in temporal lobe epilepsy: Voxel-wise and numerical analysis – Daichi Sone (United Kingdom)
Neuropsychology
Chair: Mary Lou Smith (Canada)
194 Impoverished future thinking in TLE: a novel cognitive deficit in epilepsy and its implications for surgical counselling – Genevieve Rayner (Australia)
212 Childhood Trauma Profiles in Epilepsy and Psychogenic Nonepileptic Seizures – Tianren Yang (Australia)
502 Randomized Controlled Trial on Neuropsychological Rehabilitation for Patients with Drug Refractory Epilepsy: Challenges, Adaptations & Findings – Shivani Sharma (India)
Paediatric epileptology 1
Chair: Elissa Yozawitz (USA)
1163 Telemedicine, health disparities and seizure control in pediatric epilepsy during the COVID-19 pandemic – Michael Kaufman (USA)
432 The Role of Neuropeptides in Electrical Status Epilepticus During Slow Sleep – Miray Atacan Yaşgüçlükal (Turkey)
467 Post-Operative Outcomes of Epilepsy Surgery in Drug Refractory Pediatric Epilepsy From Western India – Mayur Thakkar (India)
611 Severe complications of influenza infection in SCN1A-Dravet syndrome – Katherine Howell (Australia)
Paediatric epileptology 2
Chair: Pauline Samia (Kenya)
999 Comparison of Efficacy of Low Glycemic Index Therapy and Modified Atkins Diet in children with DRE: A Randomized Non-inferiority Trial – Vaishakh Anand (India)
1140 Felbamate role in intractable pediatric epilepsy- should we keep on using it as the last resort? – Shira Rabinowicz (Israel)
836 The natural history of SCN8A epilepsy and related diseases – Elena Gardella (Denmark)
Social issues/nursing & Pandemic response
Chair: Jacob Mugumbate (Zimbabwe)
231 The Ottawa Epilepsy Program: region-wide coordinated and community integrated care in the 21st century – Tadeu Fantaneanu (Canada)
091 Employment in people with epilepsy: A cross sectional study – M. H. Holy Chan (Hong Kong)
496 COVID-19 pandemic in Istanbul: Seizure Frequency and Psychosocial Outcomes in Patients with Epilepsy – Kubra Yeni (Turkey)
943 Multi-centre development of a secure, cloud based, patient to clinician, neurology video transfer, classification and management system – Sameer Zuberi (United Kingdom)
Status epilepticus
Chair: Eugen Trinka (Austria)
700 Status epilepticus outcome in patients with and without MRI abnormalities – Pilar Bosque Varela (Austria)
539 Temporal Trends in Hospital Admissions and Incidence of Status Epilepticus and Epilepsy in England 2003- 2018 – Aidan Neligan (United Kingdom)
242 The 2HELPS2B scale is useful to predict the prognosis and development of epilepsy in encephalopathic patients with suspected status epilepticus – Jordi Ciurans Molist (Spain)
968 Metformin protects rats against Status Epilepticus associated Cognitive dysfunction by ameliorating neuroinflammation and neuronal death – Sree Lalitha Bojja (India)
An international classification of cognitive disorders in epilepsy: the IC CoDE
This workshop will introduce the International Classification of Cognitive Disorders in Epilepsy (the IC CoDE) project to the wider epilepsy community. This is a project in development and feedback is required from clinicians and researchers to ensure it is on the right track, to secure ‘buy in’ once the classification system is launched.
Brief (7 minute) presentations from the speakers will present the background and rationale for the project and progress to date. Small discussion groups, each moderated by a YES member from different regions of the world, will be used to create challenges to the model and discuss difficulties in implementing a single diagnostic system across epilepsy syndromes, across international borders and across clinical and research settings. The outcomes of these discussions will then be synthesised by the moderators who will provide feedback in a plenary session at the end of workshop.
It is intended to write up the proceedings of the workshop and the outcomes of the discussion will inform the development of the classification. Interested participants in the workshop will all be sent this summary and will be invited to join the wider consultation group for the project as it moves into its final stage of development.
Chair: Sallie Baxendale (United Kingdom)
- Carrie McDonald (USA)
- Bruce Hermann (USA)
- Sarah Wilson (Australia)
Case studies in pregnancy and epilepsy
Specific Aims:
- Detail appropriate pre-pregnancy counselling and management;
- Review management of epilepsy in pregnancy and postpartum;
- Highlight important unanswered questions and needed future research directions.
Learning Objectives:
- Understand appropriate pre-pregnancy counselling and management;
- Improve approaches to management of epilepsy in pregnancy and postpartum;
- Comprehend important unanswered questions and needed future research.
Chair: Kimford Meador (USA)
- Case related to pre-pregnancy counselling and management – Torbjörn Tomson (Sweden)
- Case related to management of epilepsy in pregnancy and postpartum – Page Pennell (USA)
- Case related to important unanswered questions and needed future research – Piero Perucca (Australia)
Changing driving policies – an interactive session
In this session, we will address key elements that influence epilepsy related driving policies. First we will discuss risk assessment and how it influences driving recommendations. Second, we will discuss how to change driving policies – i.e. the practical approach to achieving this important goal. Then we will discuss next steps when it comes to driving and epilepsy. Finally we will make concluding remarks. By the end of the session, participants will be familiar with elements that influence driving policy including driving risk and approaches to successfully working with regional/national stakeholders to change driving policies.
Chair: Nathalie Jette (Canada)
- Introduction - Nathalie Jette (USA)
- Risk assessment and how does it influence driving recommendations? – discussion - Ettore Beghi (Italy)
o How to assess driving risk in people with epilepsy - Alejandro de Marinis (Chile)
- How to influence driving regulations and legislation – discussion - Amza Ali (Jamaica)
o How to influence driving regulations and legislation: the Austrian experience - Christoph Baumgartner (Austria)
o How to influence driving regulations and legislation: the Japanese experience - Takuji Nishida (Japan)
- Next steps – discussion - Mary Secco (Canada)
o Where do we go next to remove barriers to driving in those with epilepsy who are well controlled, etc. - Michael Sperling (USA)
- Conclusions/final discussion - Alejandro de Marinis (Chile)
Connectomics in epilepsy
This highly interactive session will be divided into four 15-minute presentations. The first presentation will be a basic introduction to connectomics, which will serve as a foundation for the subsequent presentations. The second presentation will focus on basic evidence of network reorganization in focal epilepsy and how it can evolve over time and potentially influence presurgical workup of persons with drug resistant epilepsy. The third presentation will review how connectivity can be used to probe cognitive networks and dysfunction in epilepsy. Lastly, an interactive wrap up and Q&A session will be held.
Aims:
Connectomics 101:
- To overview the available techniques to map brain networks in the healthy and epileptic brain
- To give a very brief introduction on how we can analyze these networks formally
Network reorganization and treatment outcomes in focal epilepsy:
- To introduce evidence that networks evolve over years of epilepsy duration.
- To introduce evidence that networks can inform epilepsy treatment outcomes.
Cognition in epilepsy: towards a network perspective:
- To show that cognitive function can be mapped via network-based approaches
- To highlight key examples of network abnormalities underlying cognitive impairment in common epilepsies
Co-chairs: Paolo Federico (Canada) & Boris Bernhardt (Canada)
- Connectomics 101 – Sara Lariviere (Canada)
- Network reorganization and treatment outcomes in focal epilepsy – Victoria Morgan (USA)
- Cognition in epilepsy: towards a network perspective – Lorenzo Caciagli (USA)
- Wrap-up
Epilepsy: from big data to better data
Aims
- To provide an accurate picture of current progress in epilepsy big data efforts worldwide,
- To identify challenges and pitfalls in putting big data projects together,
- To identify a roadmap for the future of epilepsy big data, maximizing impact and learning from industry.
Learning objectives
- To learn of epilepsy big data projects worldwide and their impact on the field,
- To learn about the challenges of big data enterprises in epilepsy
- To learn how individual clinicians and researchers can contribute to big data efforts, and
- To learn what the future may bring to the field through big data research and clinical collaborations.
Chair: Samden Lhatoo (USA)
- Philippe Ryvlin (Switzerland)
- Vikram Rao (USA)
- Sam Berkovic (Australia)
- Sanjay Sisodiya (United Kingdom)
Epilepsy and intellectual disability – best papers
The session will feature major advances in different fields of epileptology like diagnostics, drug therapy, surgery, and many more, tailored to the associations between epilepsy and ID. This often neglected field is now in the focus of science because first steps of personalized medicine in epileptology have their origin here. The audience will learn about recent progress for persons with ID and in addition to this about general principals and achievements for epileptology as a whole.
Chair: Christian Brandt (Germany)
- Danielle Andrade (Canada)
- Laura Guilhoto (Brazil)
- Candan Gurses (Turkey)
- Kousuke Kanemoto (Japan)
- Mike Kerr (United Kingdom)
- Christine Linehan (Ireland)
- Francis Tan (Netherlands)
- Vicente Villanueva (Spain)
Facilitating research in resource poor settings: the Fogarty Program
This session will disseminate information about research funding opportunities and mentoring. There will be discussion about how successful applicants went about building the projects, with information about requirements and the process.
Co-chairs: Edward Bertram (USA) & Angelina Kakooza-Mwesige (Uganda)
- Kathleen Michels, Fogarty International Center, NIH (USA)
- Suzan Nadi, Center for Scientific Review, NIH (USA)
- Angelina Kakooza-Mwesige, Makerere University (Uganda)
- Edwin Trevathan, Vanderbilt Institute of Global Health (USA)
Is this a spike? Or not? Operational criteria for epileptiform EEG discharges
Operational criteria for defining and identifying interictal epileptiform discharges have been recently proposed and validated in several studies. The learning objective of this interactive session is to teach the audience these criteria. At the end of the session, the participants will be able to apply these criteria in their clinical practice. Overreading of EEG is the most common cause of misdiagnosing epilepsy, therefore this topic is important to improve the care of patients with seizures, paroxysmal events and suspected epilepsy.
Chair: Sándor Beniczky (Denmark)
- Is this a spike? Or not? Operational criteria for epileptiform EEG discharges – Sándor Beniczky (Denmark)
- Sándor Beniczky (Denmark)
- Fábio Nascimento (USA)
- Mustafa Aykut Kural (Turkey)
Key aspects of transitioning your patients from paediatric to adult care
Chair: Danielle Andrade (Canada)
- Introduction of the goals of ILAE Transitions from Child to Adult Care Task Force – Danielle Andrade (Canada)
- Key aspects of transition – Rima Nabbout (France)
- Case presentation: Young patient with Juvenile Myoclonic Epilepsy: her transition issues – Jaime Carrizosa (Colombia)
- Case presentation: Young patient with developmental and epileptic encephalopathy – Danielle Andrade (Canada)
Neurostimulation and minimally invasive techniques
In this session, we will explore advanced neurostimulation strategies for drug resistant epilepsy and future directions.
Co-chairs: Dario Englot (USA) & Bertil Rydenhag (Sweden)
- Open loop hippocampal stimulation for epilepsy – Arther Cukiert (Brazil)
- Closed loop VNS for epilepsy: outcomes and future directions – Michal Tzadok (Israel)
- Closed loop thalamic stimulation for epilepsy – Rushna Ali (USA)
New neonatal seizure classification: interactive quiz
In 2021, a modification of the ILAE classification of seizures and the epilepsies was suggested for seizures in the neonate. The new framework is based on the ILAE classification for seizures and epilepsies, but takes into account specific aspects of seizures in the neonate. Since neonatal seizures may be electrographic-only, it emphasizes the role of electroencephalography in the diagnosis. The suggested classification aims to guide the clinician with regards to diagnosis, underlying etiology, and treatment.
This session aims to highlight challenges regarding diagnosis and classification of neonatal seizures from both the neonatologist’s and the epileptologist’s perspective. Examples of seizures in neonates will be presented and discussed, a quiz will allow the audience to train skills in using the classification, and gain more competence in applying it in clinical practice and research
Chair: Hans Hartmann (Germany)
-
Clinical challenges of neonatal seizures - Sudhin Thayyil (United Kingdom)
-
Challenges of diagnosing neonatal seizures - Geraldine Boylan (Ireland)
-
Introduction to the new classification - Ronit Pressler (United Kingdom)
-
Cases, quiz - Vaisakh Krishnan (India) & Hans Hartmann (Germany)
-
Discussion
Psychotherapy for psychogenic nonepileptic seizures after the CODES trial: where next?
The randomised controlled CODES study comparing Cognitive Behavioural Therapy for Dissociative (non-Epileptic) Seizures and standardised medical care with standardised medical care alone involved a total of 368 patients and set new research quality standards in the field of Psychogenic Nonepileptic Seizures (PNES). While patients in the CBT arm did better than those in the control arm in terms of the pre-defined primary outcome (seizure frequency) and in 13 secondary outcomes, the between group differences were only significant in 8 secondary outcome measures. While providing some support for the effectiveness of psychological treatment for PNES, the outcome of the CODES trial therefore raises a number of questions for the future of PNES research and service provision. In this session, members of the ILAE PNES Task Force will discuss some of these questions in a series of five minute presentations intended to engage the audience in an interactive debate about the future of psychological treatment (research) for patients with PNES. By the end of the session participants should have a better understanding of the difficulties PNES psychotherapy (research) has to overcome and some ideas how to do this.
Chair: Markus Reuber (United Kingdom)
- Key outcome of the CODES trial of CBT and standardised medical care versus standardised medical care for patients with dissociative seizures – Markus Reuber (United Kingdom)
- Psychotherapy for PNES: one for all or all for one? – Rod Duncan (New Zealand)
- How to secure an evidence base for psychotherapy for PNES? – W Curt LaFrance (USA)
- What outcomes are the most important in the treatment of PNES? – Ali Asadi Pooya (Iran)
- Psychological interventions for populations with limited access to health care resources – Chrisma Pretorius (South Africa)
- Patient empowerment and personalisation of psychotherapy – Coraline Hingray (France)
Self-management in epilepsy: time to incorporate it into your practice
Epilepsy self management extends beyond the clinic into the patients’ home and community and aims to increase patients’ skills and confidence in monitoring symptoms, problem-solving, decision-making, goal setting, communication, and adopting healthful behaviours to improve health and quality of life (Helmers et al., 2016).
Learning objectives:
- Participants will be able to identify the opportunities and barriers to providing self management programs for persons with epilepsy;
- Participants will have a better understanding of the problems that people with epilepsy have that are amenable to self-management.
Chair: Mary Secco (Canada)
- Francesca Sofia (Italy)
- Gus Baker (United Kingdom)
- Natela Okujava (Georgia)
The ketogenic diet: highlights for the centennial following its birth
To provide latest updates on the ketogenic diet and discuss a possible collaboration. Four speakers will share cases and talk about their topics. Each talk will be followed by an interactive live polling and discussion on topics related to the cases.
Co-chairs: Heung Dong Kim (Korea, Republic of) & Jong Rho (USA)
- Myoclonic astatic epilepsy and the use of the ketogenic diet – Christina Bergqvist (USA)
- Efficacy of the ketogenic diet in genetic epilepsies – Sehee Kim (Korea, Republic of)
- Role of the gut microbiota in pediatric epilepsy – Jong Rho (USA)
- Application of the ketogenic diet in the treatment of refractory status epilepticus - Mackenzie Cervenka (USA)
Toward an understanding of drug resistance in epilepsy
Drug resistant epilepsy is often cited as one of the critical issues that reduces the quality of life in patients who are afflicted by incompletely controlled seizures. However, there has been very little research specifically addressing the cause(s) of drug resistance. What work has been done has been directed at overcoming one or another hypothesized mechanism. Failure of an intervention to overcome drug resistance has rarely, if ever, addressed the question whether failure was because it was the wrong hypothesis or whether the intervention did not have the desired effect, even if the theorized mechanism was correct. Progress requires a specific focus on the potential causes so that they can be directly addressed experimentally and clinically.
In this interactive session we will open the conversation about the recognized patterns of drug resistance and some of the potential contributing mechanisms. The goal of this conversation is to begin a focus in our clinical and basic science community on drug resistance to identify the causes and how they might be overcome.
The session will be organized by a working group of the ILAE/AES Joint Translational Task Force (TASK1) on “models of drug resistance”.
It will be initiated with brief overviews of the potential patterns of drug resistance in epilepsy across the lifespan, and some of the contributing mechanisms followed by an open discussion with the participants.
There will be two chairs and a panel of discussants. The discussants will participate in guiding the discussion by concisely framing the background or highlighting areas of debate and by posing questions challenging current concepts to the participants.
Co-chairs: Heidrun Potschka (Germany) & Solomon Moshé (USA)
- Edward Bertram (USA)
- Matthew Walker (United Kingdom)
- Aristea Galanopoulou (USA)
- Stéphane Auvin (France)
- Luisa Rocha (Mexico)
Treatment of young children with epilepsy : OFF label use ON the table
The Medical Task Force of the ILAE Pediatric Commission wants to highlight the need for more clinical trials and better regulatory approval policies for young children with epilepsy. Many drugs used in clinical practice are prescribed off-label. We conducted an international survey to illustrate this very concretely: 6 typical clinical scenarios were presented and first and second line treatment was asked for. Scenarios included cases on neonatal epilepsy, West syndrome, tuberous sclerosis, Dravet syndrome, non lesional focal epilepsy. The survey was completed by >600 epileptologists worldwide.
In this interactive session, we will present the results of the survey and discuss the need for future trials. We will also address which steps are necessary to change the frequent off-label use of anti-seizure medications in young children. After a short introductory lecture on the development of new anti-seizure drugs in young children, participants will be asked to debate on the results of each of the 6 scenarios and give ideas about future steps in research and policy making.
Learning objectives
- understand the typical pathway to develop new anti-seizure medications in children
- understand the first and second line treatment options in infant and childhood epilepsies
- help to design future trials in young children with epilepsy
Chair: Lieven Lagae (Belgium)
- Development of anti-seizure drugs in young children: current state and future directions – Stéphane Auvin (France)
- Presentation and Discussion: Results of international ILAE survey on first and second line drugs in typical epilepsy syndromes in young children – Jo Sourbron (Netherlands) & Lieven Lagae (Belgium)
Subscribe to the ILAE Newsletter
To subscribe, please click on the button below.
Please send me information about ILAE activities and other
information of interest to the epilepsy community